MediPro Blog
The Case for Outsourcing Medical Billing: Streamlining Your Practice for Success
In the dynamic landscape of modern healthcare, medical practitioners are...
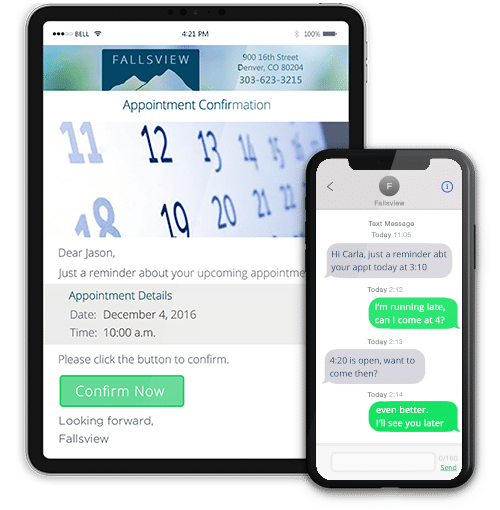
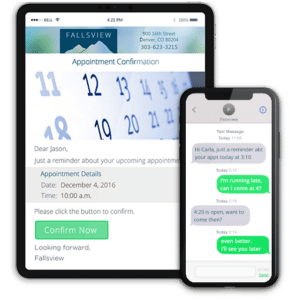
Read MoreEnhancing Patient Care: Why Medical Practices Should Embrace Patient Communicator
In today’s rapidly evolving healthcare landscape, effective communication between medical...
Read MoreEnhancing Patient Engagement
With the healthcare marketplace rapidly changing, it is of the...
Read MoreThe Patient Experience
The Pandemic Push With the emergence of the Covid pandemic,...
Read MoreA Look At Cybersecurity Threats in the Healthcare Industry
A look at cybersecurity threats in healthcare Increased and imminent...
Read MoreStrategies to Improve Patient Collections
According to experts, hospitals, and private practice that do not...
Read MoreTelemedicine and its Role in Revolutionizing Healthcare
Technology has become a centralized component of operation across all...
Read MoreMaintaining Cyber Security in a Small Medical Office
In this article, we would like to discuss an important...
Read MoreBuying EHR Systems – Make Training a Purchasing Factor
How to Assess EHR / EMR Systems Training and Implementation...
Read MoreIn-house vs. Outsourcing Medical Billing
Pros and Cons of Medical Billing Solutions Outsourcing your medical...
Read MoreMedical Billing Services 2019
Medical Billing Services 2019 For smaller medical practices and clinics,...
Read MoreMedical Billing Software 2019
Medical Billing Software Learn about the advantages of using medical...
Read MoreElectronic Health Records Errors – How to Avoid HIPAA Trouble
HIPAA Trouble and EHR Implementation – How to Avoid Legal,...
Read MoreMedical Revenue Cycle Management
Revenue Cycle Management Revenue Cycle Management is a key part...
Read MoreLytec 2020 Upgrade – New Features and More Benefits
Lytec 2020 – The Best Medical Practice Software Lytec© 2020...
Read MoreEHR Medical Software Programs
CureMD Electronic Healthcare Records Software This article provides an overview...
Read MoreEMR Security, Privacy and HIPAA Compliance
Protecting Electronic Medical Records and Medical Practice Liabilities EMR discussions...
Read MoreAdvantages and Disadvantages of EMR vs. Paper-Based Records
Electronic Medical Records vs. Paper-Based Records This article presents the...
Read MorePractice Management Software Features
What Is Practice Management Software? Medical practice management software (PMS)...
Read More